What does an Out-of-Pocket Maximum Mean?
When it comes to health insurance, one of the most important terms you’ll encounter is the out-of-pocket maximum. But what does it actually mean?
In simple terms, your out-of-pocket maximum (often called “OOP max”) is the most money you’ll ever have to pay in a single year for covered healthcare services. Once you hit that limit—by paying for deductibles, copayments, and coinsurance—your insurance will cover 100% of your in-network, covered medical costs for the rest of the year.
This limit is your financial safety net. It protects you from huge medical bills if you face a serious illness, surgery, or emergency.
For example, in 2022, the federal limit for Marketplace plans was $8,700 for an individual and $17,400 for a family. Once your expenses reach those amounts, your plan steps in to pay everything else for the rest of the year.
Why the Out-of-Pocket Maximum Matters
Without a limit, medical costs could spiral out of control—especially during a major health event. Your out-of-pocket maximum ensures that you know the most you might ever spend, providing financial predictability and peace of mind.
However, there’s a catch: not all costs count toward this limit. Understanding what’s included—and what isn’t—can save you from unpleasant surprises later.
What Counts Toward the Out-of-Pocket Maximum?
Here’s what typically does count toward your out-of-pocket maximum:
- Deductibles: The amount you pay before your insurance begins to cover costs.
- Copayments: Fixed fees for doctor visits, prescriptions, or specialist care.
- Coinsurance: The percentage you pay for services after meeting your deductible.
These expenses add up over the year until you reach your out-of-pocket maximum.
❌ What Doesn’t Count
Some payments don’t count toward this limit, including:
- Your monthly premium (the amount you pay to keep your insurance active)
- Costs for services not covered by your plan
- Charges from out-of-network providers (unless your plan specifies otherwise)
- Amounts above the “allowed” cost your insurer agrees to pay
👉 Example:
If you pay $2,000 for an elective surgery that isn’t covered by your plan, that amount won’t count toward your out-of-pocket maximum. So even if you’ve reached your limit for covered services, you could still owe more for non-covered care.
Also Read: What is a Network Provider in Health Insurance?
🩺 Tip: Always confirm whether a procedure or provider is covered before treatment. Using out-of-network providers can significantly increase your costs.
(Source: HealthCare.gov)
Government Limits on Out-of-Pocket Maximums
The federal government sets annual limits on how high your out-of-pocket maximum can be for Marketplace health plans.
| Year | Individual Limit | Family Limit |
|---|---|---|
| 2021 | $8,550 | $17,100 |
| 2022 | $8,700 | $17,400 |
| 2025 (Projected) | Around $9,500 | Around $19,000 |
These limits may vary for employer-sponsored or private plans, but most cannot exceed the federal maximum set by law.
Choosing the Right Plan for Your Needs
Different health plans balance premiums and out-of-pocket limits in different ways.
🔹 Lower Premium, Higher Risk
- Bronze and Silver plans often have lower monthly premiums but higher out-of-pocket maximums.
- These are good for people who are generally healthy and don’t expect frequent medical visits.
🔹 Higher Premium, Lower Risk
- Gold and Platinum plans have higher monthly premiums but lower out-of-pocket maximums.
- Ideal if you have chronic conditions, need ongoing care, or simply want more predictable costs.
💡 Rule of thumb: If you expect to use medical services often, paying a bit more each month can save you a lot later.
(Source: Forbes Health)
What Are Cost-Sharing Reductions (CSRs)?
If your income falls below a certain level, you may qualify for cost-sharing reductions (CSRs) that make healthcare more affordable.
These savings are available only if you enroll in a Silver-level plan through the Marketplace.
CSRs can help by:
- Lowering your deductible (e.g., from $750 to $300 or $500)
- Reducing copayments and coinsurance
- Decreasing your out-of-pocket maximum (e.g., from $5,000 to $3,000)
Additionally, American Indians and Alaska Natives may qualify for extra cost-sharing benefits and zero-cost coverage options.
(Source: U.S. Centers for Medicare & Medicaid Services)
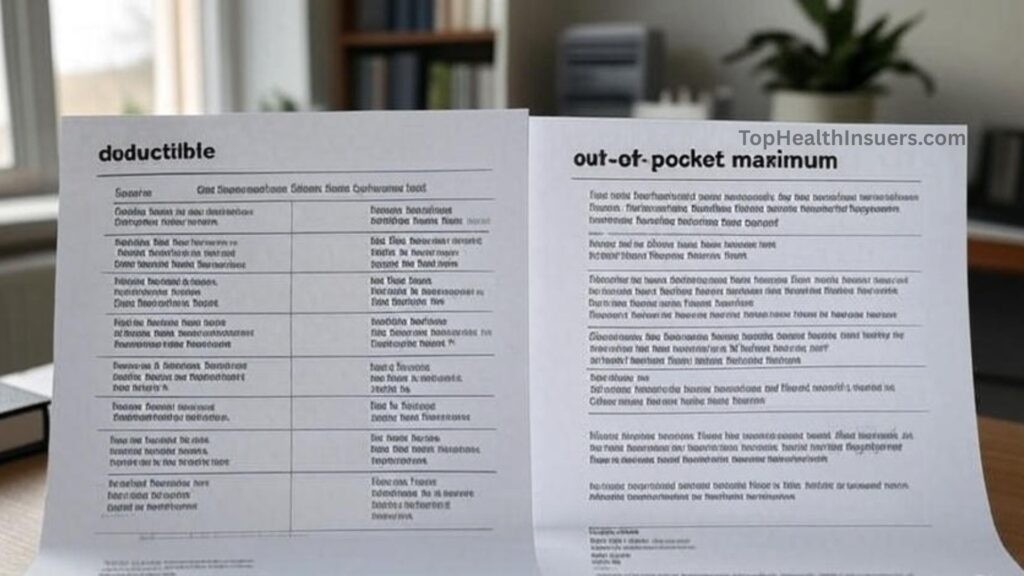
Out-of-Pocket Maximum vs. Deductible
People often confuse deductibles and out-of-pocket maximums, but they’re not the same thing.
| Term | What It Means | When It Applies |
|---|---|---|
| Deductible | The amount you pay before insurance starts covering costs. | Starts at the beginning of each plan year. |
| Out-of-Pocket Maximum | The most you’ll pay in total for covered services in a year. | Once reached, insurance pays 100% of covered expenses. |
👉 Every dollar you pay toward your deductible, copayments, and coinsurance counts toward your out-of-pocket maximum.
Once you reach it, you stop paying for covered in-network care for the rest of the year.
Also Read: How does an HMO differ from a PPO plan?
Example: How It Works in Real Life
Let’s break it down:
- Out-of-pocket maximum: $6,000
- Deductible: $4,500
- Coinsurance: 40%
Now imagine you need surgery that costs $10,000.
- You first pay your $4,500 deductible.
- You owe 40% coinsurance on the remaining $5,500, which is $2,200.
- That totals $6,700, but since your out-of-pocket max is $6,000, you only pay $1,500 more.
- Your insurance covers everything else—plus 100% of future covered services for the rest of the year.
This example shows how your OOP max caps your total expenses and keeps your healthcare costs predictable.
Key Takeaways
- Your out-of-pocket maximum limits how much you’ll pay each year for covered services.
- After you hit the limit, insurance covers 100% of covered in-network costs.
- Premiums and non-covered services don’t count toward this limit.
- Choosing the right balance between premium and OOP max depends on your health and budget.
- Cost-sharing reductions can lower your expenses if you qualify.
Conclusion: Protect Yourself from Unexpected Costs
Your out-of-pocket maximum is one of the most important protections in your health insurance plan. It ensures that no matter how many medical bills you face, there’s a limit to how much you’ll pay out of pocket.
Understanding how it works helps you choose a plan that matches your health needs and financial comfort zone.
When comparing plans, don’t just look at the monthly premium—consider your deductible, coinsurance, and out-of-pocket maximum together.
Pro Tip: Always review your Summary of Benefits and Coverage (SBC) before enrolling. It clearly lists your deductible, copays, coinsurance, and out-of-pocket max.
FAQs About Out-of-Pocket Maximums
Q1. Does my premium count toward my out-of-pocket maximum?
No. Premiums are separate from your OOP max and don’t count toward it.
Q2. Do out-of-network costs count toward my OOP maximum?
Usually not. Most plans only apply in-network expenses to your OOP max.
Q3. Can I reach my out-of-pocket maximum without meeting my deductible?
Yes, it’s possible. Your deductible, copays, and coinsurance all contribute to your total OOP spending.
Q4. What happens after I reach my out-of-pocket maximum?
Your insurer pays 100% of covered, in-network medical expenses for the rest of the plan year.
Q5. Can my out-of-pocket maximum change each year?
Yes. Federal limits and plan designs may adjust annually.

Post Comment